One of the most common problems of the spine is non -specific pain in the back of the back.According to the National Health Statistics Center, 26-32% of the adult population suffers from chronic lower back pain.Osteochondrosis is a common cause of such pain.
Osteocondrosis is the early wear and aging of intervertebral discs and vertebrae.Osteochondrosis can occur at any part of the spine: cervix, chest, groin or groin.The lumbar segment is most often affected and the lumbar osteochondrosis develops.If they do not start treating in time, the disease can affect several classes at a time.
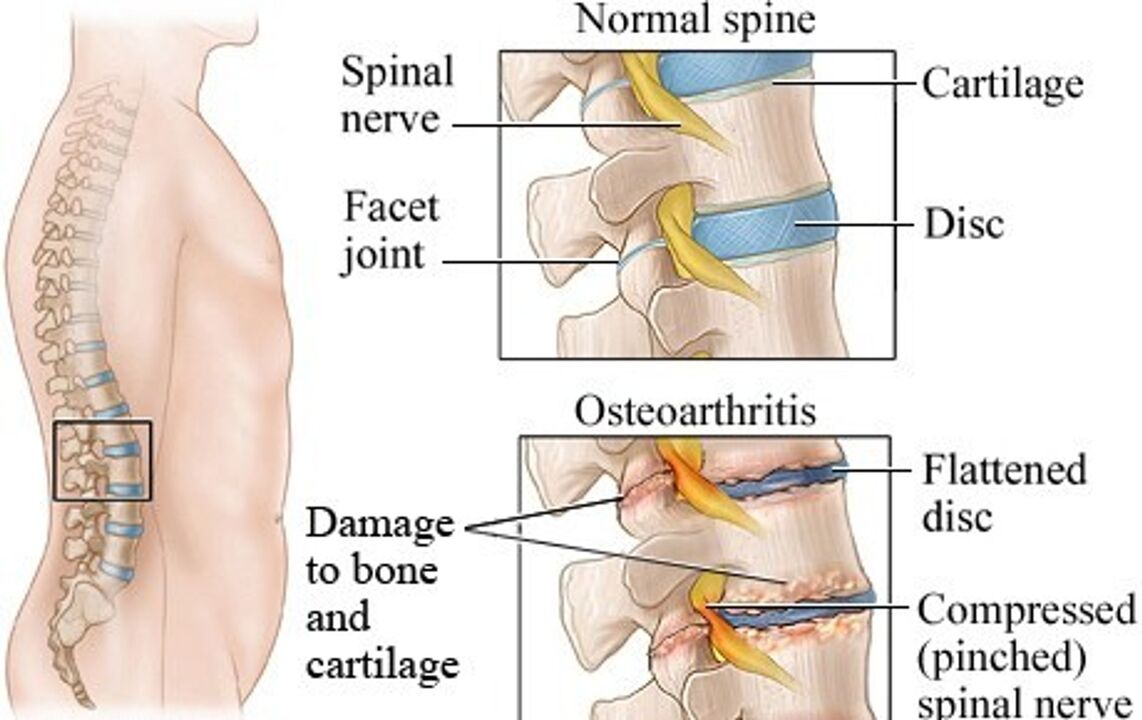
The lumbar region of osteochondrosis is a chronic degenerative disease in which the cartilage tissue of the lumbar disks is destroyed in the lumbar region.There are two main parts on the intervertebral plate: the core and the fibrous ring.With increased load, these structures are destroyed, leading to the compression of the nerves and the appearance of acute pain.
As the disease develops slowly, its signs are at first difficult to notice.The patient does not pay attention or does not understand exactly where it hurts.As a result, they often arrive at the doctor when the intervertebral hernia develops.
Causes of osteochondrosis
Lumbar osteochondrosis, as most diseases of the muscle bone system, has non-infectious etiology.The risk factors for the development of osteochondrosis are primarily due to a person's motor activity, lifestyle, professional working conditions and inheritance.Be the main and perhaps the most important factors.
Violation of posture and reducing motor activity- Given the modern rhythm of life, people have to be in the same position for a long time, like office work, driving or studying.Because of this, many people have problems with posture, including skoliosis.When the posture is interrupted, the load on the spinal column is unevenly distributed: some discs are loaded better than others.The lumbar region suffers more than others.And for the lumbar class, this load is often more than other classes.
Excessive physical activity- If someone does not play sports and the back muscles are weak, intense workout can hurt.Practices related to additional burdens and excessive load on the lumbar region lead to injuries, and intervertebral plates wear prematurely.
Body weight and obesity are superfluousIncrease the axial load on the spine.At the same time, the nutrition of intervertebral discs is interrupted, which causes the dystrophic processes to develop.
Age -related changes- After 60 years, tissue recovery processes slow down, so in older people the likelihood of a higher level of hernia between the vertebrae.
Hereditary factors- If a person is naturally confused by the properties of cartilage and bone tissue, then osteochondrosis will develop earlier and progress will be faster.
The first signs and main symptoms of lumbar osteochondrosis
Intervertebral discs soften the shocks while walking, running and jumping.This function suffers from structural changes accompanying lumbar osteochondrosis.
When the intervertebral discs of osteochondrosis become thinner, this leads to an increase in vulnerability of nerves and blood vessels.The nerves are pinched and their nutrition is disturbed, acute pain and other symptoms of lumbar osteochondrosis.
Sharp and chronic lower back pain- This is the main complaint of lumbar osteochondrosis.Personal activity, hypothermia, uncomfortable pose can cause pain.Occasionally, the pain is all back and the feet.
Tingling, burning and numbness (paresthesia) in the lower and legs-The lumbar osteochondrosis symptoms that appear due to the compression of the nerves.
Increase the sound of the back muscles in the lumbar regionIt increases pain and can lead to a reduction in mobility.
Stages of lumbar osteochondrosis
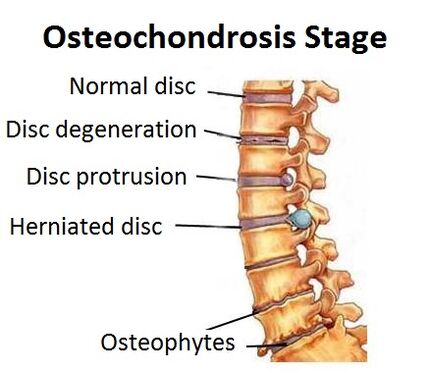
Changes in cartilage and bone tissue occur slowly.Depending on the prevalence of the pathological process, four stages of lumbar osteochondrosis are distinguished.
Stage 1- This is the beginning of the disease (chondrosis).The location of the sheet gelatin core changes relative to the fibrous ring fibers.This leads to irritation of nerves and pain.Sometimes nothing hurts at this stage.
Section 2- Due to the displacement of the discs, the intervertebral gap decreases and cracks appear in the discs.The nerves are squeezed and the patient suffers from acute lower back pain.
Section 3- The intervertebral discs are completely damaged and a fibrous ring is destroyed.At this stage, there is a high risk of developing vertebrae.The pain increases, appears more often, and is different: acute and chronic pain.
Stage 4- The disease applies to nearby tissues.In the lumbar region, mobility is reduced, and pain even occurs with minor changes in the body position.At this stage, the intervertebral hernia develops and the risk of compression of nerves and blood vessels is high in the lumbar region.
Diagnosis of lumbar osteochondrosis
If the acute lower back pain is tortured both while moving and at rest, the numbness of the legs - contact a neurologist.It performs control, determines the probable cause of pain and requires the necessary diagnosis.
The main research methods are radiography and tomography.
- Vision, observation and functional radiography of the spine in two projections.This method allows for evaluation of the state of the spine, but the soft tissues (such as muscles) and the cartilage do not appear in the images.
- Computer tomography allows you to obtain additional information as the images are received in different forecasts.Based on the results of the examination, the doctor may determine the degree of damage to the lumbar spine.
- Magnetic resonance imaging is the exact diagnosis of "gold standard" for "lumbar osteochondrosis".According to MRI, the doctor can evaluate the condition of soft tissues and identify the hernia between the vertebrae.
Treating lumbar osteochondrosis
After the diagnosis, the neurologist chooses treatment separately.This depends on the stage of the disease and the severity of the symptoms.Most patients are assisted by comprehensive conservative treatment (medication, physiotherapy exercises, physiotherapy).If the patient is not better and serious complications develop, the operation is prescribed.
Conservative treatment
Conservative treatment tasks:
- Stop the pain.
- Reduce inflammation.
- Prevent complications.
- Reduce the load on the spine by reinforcing the muscles of the back.
- Reduce the compression of the nerves.
- In intervertebral hernia - create conditions for resorption and natural healing.
In the acute phase of the disease, the doctor primarily reduces pain and inflammation with analgesics and anti -inflammatory drugs.Subsequently, the neurologist draws an individual program consisting of physiotherapy, manual therapy and physiotherapy.
PhysiotherapyIt is based on the use of physical factors: cold, heat, electric current, magnetic radiation, laser, etc.They promote pain intensity and improve tissue nutrition, which contributes to their natural recovery.
Kinin -nitherapyActive (exercise therapy) and passive (massage, adhesion).This allows you to strengthen your back muscles, relieve muscle tension, improve microcirculation and activate the recovery process.
Manual therapy and massageRemove the increased muscle tone in the lower back, restore mobility.As a result, the nutrition of the damaged area improves and the degree of nerve tightening is reduced.
GlueOr kinesiological tape glue is based on the use of elastic plasters, which are glued to the skin to weaken or improve muscle tone.Thus, the muscle frame is strengthened, in the lumbar region the microcirculation improves, and the distribution of load on the spine is normalized.
Laser therapyThis is based on low intensity laser radiation and its positive effects on cell function.This contributes to the natural restoration of intervertebral discs by improving nutrition.
Plasma therapy(PRP therapy) is a method to improve regeneration processes.The patient's purified plasma injections stimulates immunity.
Reflexotherapy, acupunctureImprove blood supply in the affected areas, reduce pain.
Shock wave therapy- This is the effect of high -frequency waves on the affected area.It stimulates the natural processes of tissue regeneration and improves tissue nutrition.
Orthopedia- Custom selection of the corset to further support the spine.Allows you to partially compensate for the load on the spine.When wearing a corset, the pain is reduced and the mobility and quality of the patient's life increases.
Lumbar osteochondrosis is a chronic disease.It is important for the patient to change his or her lifestyle and learn to live with this disease.For this, there are special education programs that can improve the quality of the patient's life.
The positive effect of conservative treatment is achieved within 2-3 months.If such treatment is ineffective, the operation is prescribed.
Operation
Minimally invasive surgical operations are carried out by developing the vertebral hernia.Choice for neurosurgery treatment is threatened with special indications, severe, threatening, patient's life.
Functioning is a complex invasive treatment method associated with the risks.During or after surgery, complications may develop.The success of treatment also depends on postoperative rehabilitation, which includes the methods of conservative therapy and orthopedic correction.
Do not postpone treatment
Lumbar osteochondrosis is a progressive disease.If it is not detected on time and is not to be treated, it can lead to disability and a reduction in quality of life.Over time, it affects several parts of the spine, and acute pain becomes chronic.
Timely prevention of symptoms and treatment of lumbar osteochondrosis in the initial stages can prevent the disease and deteriorate the condition.























